Sep 15 2020
Thermography has been an interesting topic in 2020 because of the requirement for faster diagnostics to identify and prevent the spread of the ongoing COVID-19.
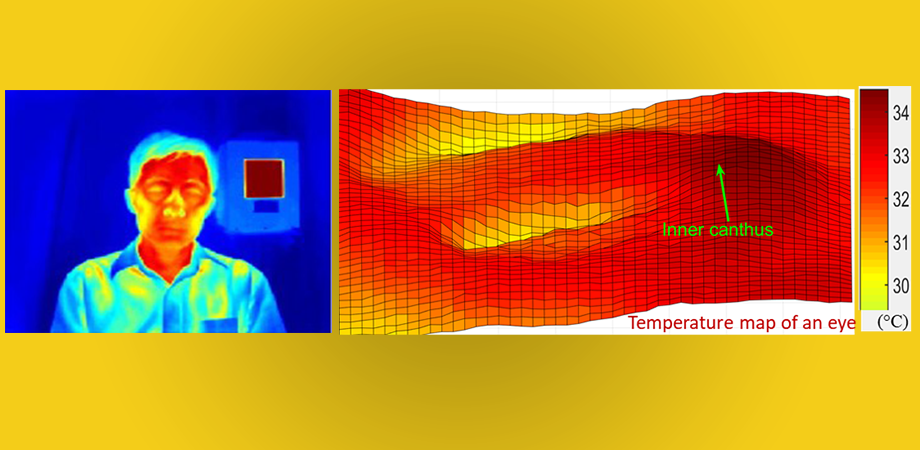 Thermal image of FDA scientist Q. Wang, with temperature map of an eye. Image Credit: Q. Wang.
Thermal image of FDA scientist Q. Wang, with temperature map of an eye. Image Credit: Q. Wang.
At present, non-contact infrared thermometers (NCITs) are a crucial tool for screening fever. However, their extensive use has been prone to imprecision.
An associated medical technology—thermography utilizing infrared thermographs (IRTs)—provides more options to estimate temperatures with higher precision.
While the use of thermography as an independent detection technique for COVID-19 may not prevent the spread of this disease, emerging proof and international consensus suggest that IRTs could be effectively utilized for detecting high body temperatures.
Published in the Journal of Biomedical Optics, a new report offers a deeper understanding of improving IRT-based fever screening. The study, carried out by Quanzeng Wang and colleagues, at the Center for Devices and Radiological Health of the US Food and Drug Administration (FDA), assessed the application of IRTs under standardized conditions.
The researchers analyzed clinical data for more than 500 demographically diverse persons, including 47 subjects with high oral temperatures (>37.5 °C), correlating facial temperatures to oral under-the-tongue thermometer measurements.
The research group verified the utility of internationally recognized (ISO) standards to acquire reliably precise results and particularly reported the efficacy of ISO techniques, such as facial area targets.
How do IRTs Work?
Humans radiate heat in the form of infrared energy, which varies as individuals get warmer. IRTs are essentially camera systems that have the ability to perceive infrared energy, enabling humans to “see” the infrared waves. Such readings display as a 2D temperature distribution that corresponds to temperature levels at the source.
Normally, a human face exhibits varying temperatures, warmer where the larger arteries are more proximal to the skin’s surface, such as the temples and inner canthi (the eye corners where the tear ducts are located).
Optimizing IRTs
Similar to any other technology, IRTs are subject to basic device and performance variations, which may have an impact on the overall precision when utilized in medical practice.
To reduce these variations, Food and Drug Administration (FDA) scientists integrated the ISO guidelines in their experiments (for example, regulating ambient conditions, requiring people to acclimatize for 15 minutes before screening, etc.).
The team reported remarkable IRT performance with distinct correlations between oral temperature baseline data and IRT readings.
Apart from presenting the effectiveness of standardized techniques for fever screening, a few major insights emerged from the group’s analysis.
One of the most considerable insights was that targeting the entire face for temperature screening led to greater precision when compared to narrowly targeting the inner canthi, as suggested by the ISO guidelines.
Such an insight can help determine future directions with such devices, since full-face imaging is relatively easier to apply because it does not need complicated facial feature detection software to recognize the inner canthi areas.
The next-best performance comprised the extended inner canthi region that includes but is broader than the inner canthi areas suggested by the ISO guidelines. Focusing on the narrow canthi areas generated third-best precision.
FDA scientists computed a range of cutoff levels to improve the specificity and sensitivity values of the IRT readings.
While no uniform consensus is available on the range of temperature that constitutes a fever, an oral temperature ranging from 37.5 °C to 38 °C (99.5 °F to 100.4 °F) is most often used in the medical profession as the threshold.
The study’s authors, however, warned that establishing a suitable cutoff temperature for real-world fever screening involves intricate considerations, like the possible rate of false positives or negatives, and also other matters like staffing, asymptomatic illness, delay times, and associated costs to health agencies.
IRT-Based Fever Screening
If carried out as per the standardized protocols to guarantee precision, IRT-based fever screening may effectively detect individuals who have increased body temperatures, such as low-grade fevers (oral temperature ≥37.5 °C) related to early-stage infections and moderate symptoms.
IRT-based fever screening, especially in regard to addressing COVID-19, should be one element in a multilayered diagnostic process that would include other helpful tools. When used in combination with other diagnostics and medical screening it is a much more useful tool in detecting those who are ill.
Zane Arp, Director of the Division, Biomedical Physics, Food and Drug Administration
Especially for COVID-19, the FDA has published fact sheets relating to the correct use and restrictions of such systems.
Considering the potential value of IRTs for medical diagnostics, improving IRT-based fever screening is very crucial, yet there remains much to learn. Wang added that the FDA team has planned further analysis to evaluate the potential effect of these factors as intersubject and environmental variability.
Journal Reference:
Zhou, Y., et al. (2020) Clinical evaluation of fever-screening thermography: impact of consensus guidelines and facial measurement location. Journal of Biomedical Optics doi.org/10.1117/1.JBO.25.9.097002.