Apr 8 2014
Each year prostate tissue samples are taken from over a million men around the world – in most cases using 12 large biopsy needles – to check whether they have prostate cancer. This medical procedure, which was recently described by an American urology professor as 'barbaric'**, shows that 70% of the subjects do not have cancer.
The examination is unnecessarily painful and involves risk for these patients, and it is also costly to carry out. A patient-friendly examination, which drastically reduces the need for biopsies, and may even eliminate them altogether, has been developed at Eindhoven University of Technology (TU/e), together with AMC Amsterdam. The results will be presented at the European Association of Urology Congress in Stockholm, on 14 April.
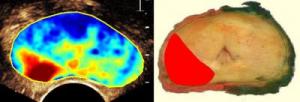 This is a prostate image made with Contrast Ultrasound Dispersion Imaging and a photo of same prostate (after surgical removal) with cancerous area colored red. Credit: Eindhoven University of Technology
This is a prostate image made with Contrast Ultrasound Dispersion Imaging and a photo of same prostate (after surgical removal) with cancerous area colored red. Credit: Eindhoven University of Technology
Hundreds of thousands of men die each year from prostate cancer. The standard procedure used worldwide for prostate cancer examinations starts with measurement of the PSA (prostate specific antigen) value in the blood. If this is high, physicians will usually remove samples of prostate tissue through the anus at six to sixteen points for pathological examination. However, 70% of the subjects show no signs of cancer. So does this mean the high PSA level is a false alarm? Not always: the biopsies may have been taken at just the wrong places. Cancer is later found in 30% of the patients with negative results (no cancer). Among the positive results (patients with signs of cancer), doctors do not know the exact sizes of the tumor. In many cases, operations show that the tumors are so small that surgery was unnecessary. As well as that, the examination leads to inflammations in up to 5% of patients. Plus the fact that each examination costs around USD 2500 to carry out.
Recognizable blood vessel pattern in cancer
Research team leader Massimo Mischi at TU/e has developed a method to investigate whether and where men have prostate cancer using existing ultrasound scanners, together with the Academic Medical Center Amsterdam. These devices create images of organs in the body using sound waves, in the same way as prenatal ultrasound scans. But these systems are usually unable to show the difference between healthy and tumor tissue. To make this visible, Mischi used the fact that tumor tissue produces large numbers of small blood vessels to allow it to grow, with a characteristic pattern. Patients are given a single injection of a contrast medium containing tiny bubbles, which are shown by the ultrasound scanner right down to the smallest blood vessels. Using advanced image-analysis techniques that can recognize the characteristic blood vessel pattern in tumors, the computer then generates an image showing where the tumor is. The examination only takes one minute, and the results are available no more than a few minutes later. These examinations also save money, because costly biopsy analysis is no longer necessary.
Precise prediction
The researchers were able to compare the 'tumor images' from 24 patients at three hospitals in the Netherlands with the actual prostates after removal by operation. The images were found to give a good indication of the locations and sizes of the tumors. Massimo Mischi will present the results at the European Association of Urologists Congress in Stockholm on 14 April. It is exceptional for a scientist from a university of technology to be given the opportunity to speak at this congress of medical specialists.
Far fewer biopsies
The use of the new method, which has been patented by TU/e, can avoid the need for biopsies to be taken from millions of men around the world. The procedure will no longer be necessary for a large part of the 70% of men from whom biopsies are currently taken unnecessarily. And far fewer biopsies will need to be taken from the remaining 30% because the location of the tumor is already clear. Once the new method has been sufficiently proven in clinical practice, the need to do biopsies may even be eliminated almost entirely.
Quick and simple introduction
The research is being carried out together with the Academic Medical Center Amsterdam and two other Dutch hospitals. A major comparative study will be held in these hospitals next year between the old and new methods, to proof that the new method is better. This will involve the use of both methods on at least 250 men. If all goes well the method will also be made available from 2016 for other patients, a large part of which will then no longer have to undergo the old and painful form of examination. The new method can be introduced quite simply because no new equipment is required; the existing ultrasound scanners which the hospitals already have can continue to be used.
Massimo Mischi received a Vidi grant from the NWO (Netherlands Organisation for Scientific Research) in 2009 for his research, and in 2011 he received a Starting Grant from the European Research Council. A 4-year grant for further research was provided by the Dutch Cancer Foundation (KWF Kankerbestrijding) in 2013 to the AMC and TU/e.
** Matthew Gettman, professor of urology at the Mayo Graduate School of Medicine in Rochester, MN, USA, wrote in 2012 in the journal European Urology that the method is "barbaric", despite the use of local anesthetic.