Feb 14 2017
Researchers funded by the National Institute of Biomedical Imaging and Bioengineering have developed a non-invasive imaging technique that accurately detects skin cancer without surgical biopsy. Multiphoton microscopy of mitochondria—small organelles that produce energy in cells—accurately identified melanomas and basal cell carcinomas by detecting abnormal clusters of mitochondria in both types of skin cancer.
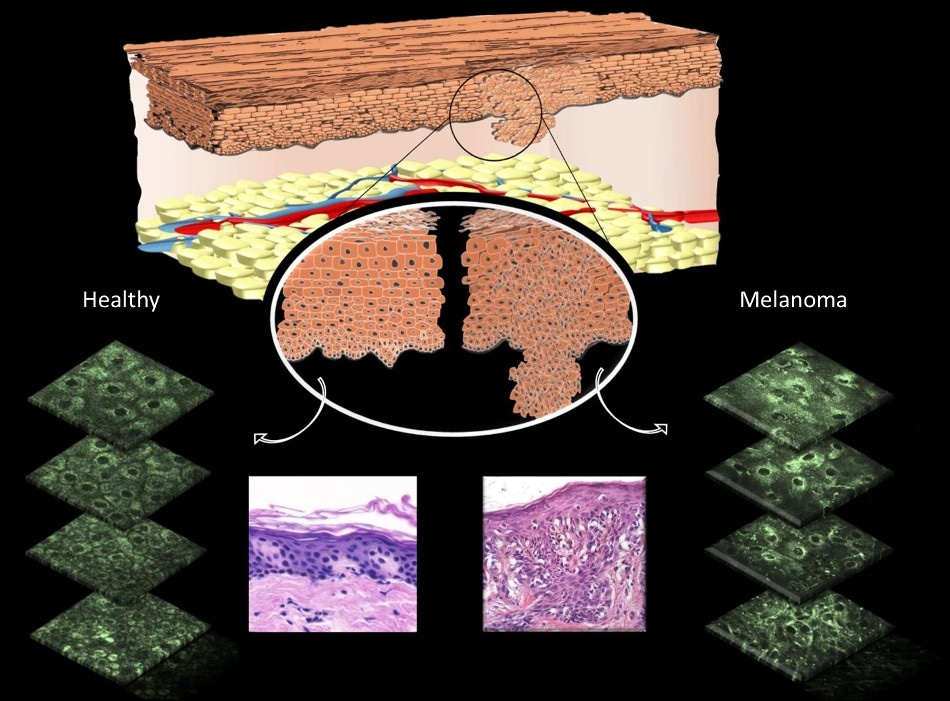 Diagram showing differences that can be observed in cell morphology in normal skin cells versus melanomas. Pink images show differences following biopsy and staining by a pathologist. Green slices show differences in fluorescence pattern of mitochondria using multiphoton microscopy. Source: Irene Georgakoudi, Tufts University.
Diagram showing differences that can be observed in cell morphology in normal skin cells versus melanomas. Pink images show differences following biopsy and staining by a pathologist. Green slices show differences in fluorescence pattern of mitochondria using multiphoton microscopy. Source: Irene Georgakoudi, Tufts University.
Skin cancer is the most common type of cancer in the U.S. and most types of skin cancer are highly treatable, especially if detected early. “The technology developed here has the potential to make the detection of skin cancers extremely rapid and feasible at very early stages,” says Behrouz Shabestari, Ph.D., director of the NIBIB Program in Optical Imaging and Spectroscopy. “Rather than taking a biopsy sample that must be processed and then examined under a microscope by a pathologist, this system involves simply looking through the microscope at the patient’s skin and determining whether it is cancerous or not, within minutes.”
A group of international collaborators led by co-senior author Irene Georgakoudi, Ph.D., in the Department of Biomedical Engineering at Tufts, found that mitochondria behave very differently in healthy versus cancerous tissue. They used a laser microscopy technique that takes advantage of the characteristics of a key molecule in mitochondria, nicotinamide adenine dinucleotide (NADH), that is central to energy production. They found that NADH, which naturally fluoresces without injecting any dye or contrast agent into the individuals being screened, can be detected using multiphoton microscopy to provide diagnostically useful information about the organization of the mitochondria in skin cells.
“The system allows us to obtain very high-resolution images of individual cells without having to slice the tissue physically,” explained Georgakoudi. “With this technique, we found that in normal cells the mitochondria are spread throughout the cell in a web-like pattern. Conversely, cancerous skin cells show a very different pattern with the mitochondria found in clumps or clusters typically at the center of the cell along the border of the nucleus.”
In this study the technique was tested in 10 patients with skin cancer (melanoma or basal carcinoma) and four who did not have skin cancer. The imaging technique results were compared to the traditional biopsy results obtained from each patient. The results demonstrated that the imaging technique correctly identified skin cancer in all 10 cancer patients, and made no false diagnoses in the four individuals without skin cancer.
Georgakoudi estimates that this test could be routinely used in doctor’s offices within five years, although the $100,000 price tag for the laser used in this microscope could limit the medical facilities that would be able to make such an investment. “Less-expensive lasers are on the horizon,” concludes Georgakoudi. “However, this approach would enable a doctor to make a quick diagnosis and begin treatment immediately, which could ultimately lower health care costs associated with these very common cancers.”
The researchers from the Department of Biomedical Engineering, Tufts University, the Laser Microbeam Program and Department of Dermatology at the University of California Irvine, the Department of Biomedical Engineering at the University of Arkansas, and the Department of Preventive Medicine in Malaga, Spain reported their findings in the November 2016 issue of Science Translational Medicine.
This research was funded by the National Institutes of Health through grant # P41EB015890 from the National Institute of Biomedical Imaging and Bioengineering. Additional funding was provided by the American Cancer Society, the Alexander S. Onassis Public Benefit Foundation, and the Arnold and Mabel Beckman Foundation.