In an article published in the journal Cancers, researchers have developed a novel portable optical polarization imaging (OPI) device for the non-invasive, rapid, and in vivo identification of basal cell carcinoma (BCC) margins.
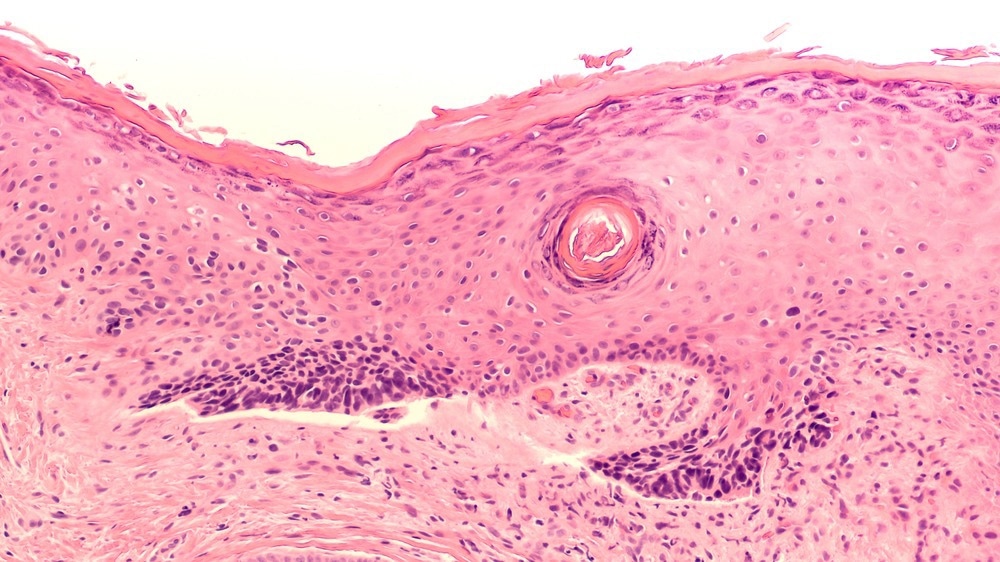
Study: Design and Validation of a Handheld Optical Polarization Imager for Preoperative Delineation of Basal Cell Carcinoma. Image Credit: David A Litman/Shutterstock.com
Due to the subtle differences between nonmelanoma skin cancer cells and healthy skin, basal cell carcinoma removal becomes a challenging procedure demanding high precision. Before Mohs surgery, 10 participants with biopsy-confirmed basal cell carcinoma were examined to test the efficiency of the portable imager.
The images gathered through optical imaging were processed using a spectral encoding technique to improve the precision of the tumor boundary delineation. The preoperative nonmelanoma skin cancer margin assessment performed by the optical polarization imager was compared to the surgeon's clinical examination and the gold standard of histopathology.
The handheld optical polarization imager had 10-times shorter acquisition times and incorporated automated optical imaging. The optical polarization imager offered twice as wide a field of view and was twice as bright.
Clinical verification showed that the optical polarization imager margin assessments were more precise than the surgeon's visual assessment. In nine out of 10 cases, the images gathered by optical imaging had a good correlation with histology.
Need for Improved Preoperative Delineation Techniques
The most prevalent form of cancer is basal cell carcinoma. Epidemiological data indicate rising incidences of basal cell carcinoma across the globe. There are currently various treatment options for basal cell carcinoma, including curettage, cryotherapy, photodynamic therapy (PDT), and radiation therapy. Excisional surgery, however, remains the most common intervention technique.
During a traditional surgical resection, the tumor is excised with a lateral clearance margin adjoining normal-appearing skin. However, there is no real-time method to assess whether or not the lesion is entirely removed. Consequently, there is a high probability that the residual tumor will remain at the excision site, making the procedure dangerous.
The Mohs micrographic surgery (MMS) procedure employs intraoperative histopathology evaluation in hematoxylin and eosin (H&E) for intraoperative nonmelanoma skin cancer margin control. It is one of the most successful procedures, with a cure rate of approximately 99%. However, MMS is not readily accessible in most dermatology surgery clinics and is expensive, labor-intensive, and time-consuming.
In recent years, several attempts have been made to enhance the preoperative delineation of nonmelanoma skin cancer using optical imaging techniques such as integrated reflectance confocal microscopy (RCM) and optical coherence tomography (OCT) systems. However, initial tumor boundary evaluations remain primarily based on visual examinations performed by the surgeon.
This paper presented an optical polarization imager for preoperative non-invasive delineation of nonmelanoma skin cancer margins. The novel handheld optical polarization imager was further tested by providing optical imaging results of 10 basal cell carcinoma cases to illustrate its potential for clinical adoption.
Designing and Testing the Device
The layout of the optical polarization imager consisted of a lamp with a filter wheel that could emit narrowband light with wavelengths of 440 nm, 570 nm, or 640 nm. The skin received light from a fiber optic ring light installed with a linear polarizer.
A 0.3X/F8 macro lens was used to capture the light reflected from the skin after passing through an analyzer. A unique, 3D-printed spacer fitted with a glass plate of 38-mm-diameter was implemented to ensure the correct optical imaging distance.
The clinical performance of the portable optical polarization imaging device was assessed by performing optical imaging on patients with basal cell carcinoma before MMS. A minimum of one basal cell carcinoma lesion with biopsy confirmation was present in all enrolled subjects and were scheduled for MMS. The surgeon used a sterile purple marker to designate the clinical margins of the excision before optical imaging. An optically transparent gel-like substance was applied to the lesion to facilitate light coupling into the skin after cleaning the treatment site with isopropyl alcohol.
The outcomes of optical imaging were evaluated against clinical H&E histopathology and compared to the surgeon's preoperative visual nonmelanoma skin cancer margin evaluation. The preoperative optical polarization imaging evaluation was deemed true negative or false negative when the spectrally encoded optical imaging showed collagen disruption within or spread outside the surgeon's marking, respectively.
The findings showed that in nine out of 10 cases, preoperative nonmelanoma skin cancer margin detection using spectrally encoded OPI coincided with the observations of clinical histopathology. Optical polarization imaging accurately demonstrated the tumor within the clinically specified limits in all six patients with negative margins following the initial Mohs excision.
Four cases necessitated >1 Mohs stage to remove the lesion because preoperative visual evaluation underestimated the lateral tumor size. In three patients with positive margins, optical polarization imaging showed the tumor expanding beyond the surgical marker.
In one case, optical polarization imaging accurately detected the positive margin. However, it incorrectly showed another region's blood vessels as nonmelanoma skin cancer. Based on the findings of the pilot investigation, handheld optical polarization imaging displayed 100% sensitivity and 86% specificity.
Novel OPI Technique Improves Preoperative Delineation of Basal Cell Carcinoma Margins
This study presented the viability of the first portable OPI prototype that could be used for rapid, non-invasive preoperative identification of basal cell carcinoma margins. The system was capable of lateral resolution of about 12 mm and wide-field (approximately 3 ´ 2 cm2) rapid image acquisition using optical imaging (5-50 ms). It was lightweight and compact and could be operated with minimum training.
Clinical testing of the prototype demonstrated its enhanced performance compared to the surgeon's preoperative visual examination of lateral nonmelanoma skin cancer margins. Overall, the results showed that optical imaging of collagen had significant potential for directing nonmelanoma skin cancer treatments and enhancing their results without changing clinical procedures.
Reference
Jermain, P.R., Iorizzo, T.W., Maloney, M., Mahmoud, B., Yaroslavsky, A.N. (2022). Design and Validation of a Handheld Optical Polarization Imager for Preoperative Delineation of Basal Cell Carcinoma. Cancers, 14(16), 4049. doi.org/10.3390/cancers14164049
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.