The laboratories of Dr. Silvia de Santis and Dr. Santiago Canals, both of the Institute of Neurosciences UMH-CSIC (Alicante, Spain), have used diffusion-weighted magnetic resonance imaging to show brain inflammation for the first time and in considerable detail.
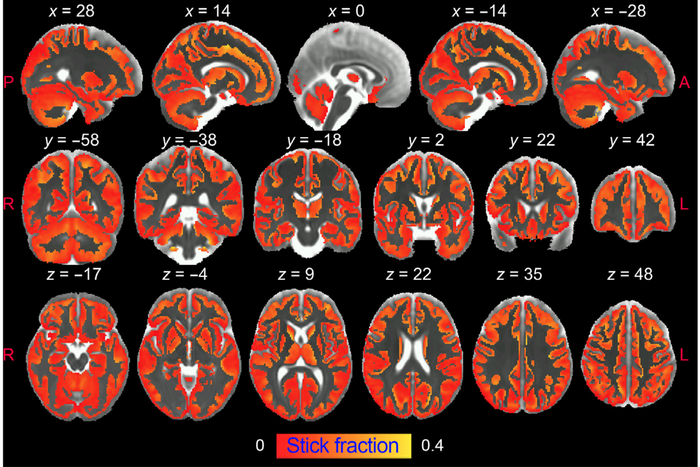 Researchers from the UMH-CSIC Neurosciences Institute have developed an innovative strategy that allows imaging of microglial and astrocyte activation in the gray matter of the brain using diffusion-weighted magnetic resonance imaging (dw-MRI). Image Credit: IN-CSIC-UMH.
Researchers from the UMH-CSIC Neurosciences Institute have developed an innovative strategy that allows imaging of microglial and astrocyte activation in the gray matter of the brain using diffusion-weighted magnetic resonance imaging (dw-MRI). Image Credit: IN-CSIC-UMH.
This comprehensive “X-Ray” of inflammation cannot be acquired using standard MRI — instead, it necessitates complex data collecting sequences and mathematical models. The scientists were able to assess the changes in the morphology of the distinct cell populations engaged in the inflammatory phase in the brain after developing the technique.
This significant achievement was made possible by the scientists’ new technique, which was released in the journal Science Advances and may be critical in changing the trajectory of neurodegenerative disease research and treatment.
The study, led by Raquel Garcia-Hernández, shows that diffusion-weighted MRI can identify the activation of microglia and astrocytes, two kinds of brain cells that are at the root of neuroinflammation and its development, noninvasively and differently.
Alzheimer’s disease and other dementias, Parkinson’s disease, and multiple sclerosis are all degenerative brain disorders that are hard to treat. Chronic inflammation in the brain is caused by the stimulation of two types of brain cells, microglia, and astrocytes, which is one of the reasons for neurodegeneration and contributes to its development.
However, there are a few non-invasive methods for identifying and quantifying brain inflammation in vivo. The current gold standard is positron emission tomography (PET), but since it is hard to generalize and is affiliated with ionizing radiation exposure, it is only used in vulnerable populations and in longitudinal studies that require PET to be used repeatedly over time, as in neurodegenerative disorders.
Another disadvantage of PET is its limited spatial resolution, which makes it inappropriate for imaging small structures. Inflammation-specific radiotracers are distributed in numerous cell types (microglia, astrocytes, and endothelium), making differentiation hard.
Despite these limitations, diffusion-weighted MRI has the unique capacity to study brain microstructure in vivo noninvasively and with high resolution by collecting the spontaneous movement of water molecules in the brain parenchyma, which generates contrast in MRI images.
Innovative Strategy
Scientists from the UMH-CSIC Neurosciences Institute have devised a novel method that uses diffusion-weighted magnetic resonance imaging (dw-MRI) to image microglial and astrocyte activation in the grey matter of the brain.
The researchers point out, “This is the first time it has been shown that the signal from this type of MRI (dw-MRI) can detect microglial and astrocyte activation, with specific footprints for each cell population. This strategy we have used reflects the morphological changes validated post-mortem by quantitative immunohistochemistry.”
Researchers also demonstrated that this method is sensitive and specific for identifying inflammation with and without neurodegeneration, allowing them to distinguish between the two diseases. It also allows doctors to distinguish between inflammation and demyelination, which are both symptoms of multiple sclerosis.
This research was also able to show the approach’s translational utility in a group of healthy humans at a full definition, “in which we performed a reproducibility analysis. The significant association with known microglia density patterns in the human brain supports the usefulness of the method for generating reliable glia biomarkers.”
We believe that characterizing, using this technique, relevant aspects of tissue microstructure during inflammation, noninvasively and longitudinally, can have a tremendous impact on our understanding of the pathophysiology of many brain conditions and can transform current diagnostic practice and treatment monitoring strategies for neurodegenerative diseases.
Dr. Silvia De Santis, Principal Investigator, Institute of Neurosciences UMH-CSIC
To test the model, the researcher utilized an established rat inflammatory model based on intracerebral lipopolysaccharide administration (LPS). In this paradigm, neuronal survival and shape are conserved while microglia (the brain’s immune system cells) are activated first, followed by an astrocyte response.
This temporal sequence of cellular events allows glial responses to be separated from neuronal degeneration and the signature of reactive microglia to be studied separately from astrogliosis.
The scientists repeated the process by pretreating the rats with an inhibitor that temporarily ablates around 90% of microglia in order to isolate the imprint of astrocyte activation. They then assessed whether the model could unravel neuroinflammatory “footprints” with and without concurrent neurodegeneration using an established neuronal loss paradigm.
“This is critical to demonstrate the utility of our approach as a platform for the discovery of biomarkers of inflammatory status in neurodegenerative diseases, where both glia activation and neuronal damage are key players,” they clarify.
Finally, the researchers employed a well-established demyelination model based on focal lysolecithin injection to show that the biomarkers produced do not reflect the tissue changes seen in brain diseases.
Journal Reference:
Garcia-Hernandez, R., et al. (2022) Mapping microglia and astrocyte activation in vivo using diffusion MRI. Science Advances. doi.org/10.1126/sciadv.abq2923.