Optogenetics is an emerging field that uses light and genetic engineering to detect and control the activity of genetically modified proteins or neurons.

Image Credit: MattLphotography/Shutterstock.com
Work in optogenetics began many decades ago, however, it was considered to make its first breakthrough into mainstream neuroscience in 2002 when Zemelman and his colleagues established a method of activating groups of rhodopsin-sensitized neurons via optical stimulation. Since then, scientists have become increasingly interested in the field of optogenetics, and much research has been carried out to leverage it in numerous applications.
Optogenetics has advanced numerous applications in various sectors, from technology to agriculture. Here, we focus on how it is revolutionizing medical research to facilitate rapid diagnosis of disease and offer monitoring and novel treatment options for various diseases.
Optogenetics in Cardiology
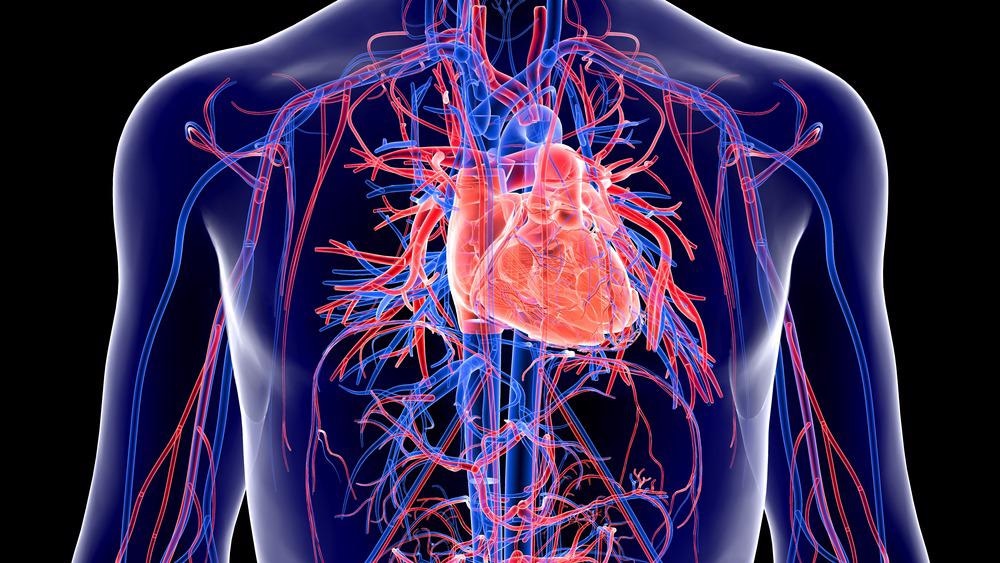
Image Credit: Shot4Sell/Shutterstock.com
Implantable ontogenetic devices are helping scientists to research cardiovascular diseases. From this, effective novel diagnostic and therapeutic approaches have been developed.
Implantable ontogenetic devices can measure various biophysical, chemical, and environmental signals. Scientists can analyze this sort of data, collected over time, to help screen for disease as well as gain a deeper understanding of how diseases emerge and progress, which leads to the development of more effective and more personalized treatment options.
In terms of cardiovascular diseases, transparent interfaces have been developed for cardiac research and have already been established as a vital tool in optical electrophysiology research. For example, one-dimensional silver nanowires (Ag NWs) and gold (Au) nanomesh have been used in variably transparent devices with excellent electrical conductivity and high degrees of mechanical flexibility. This has allowed scientists to investigate cardiovascular disease.
Wireless optogenetic devices have replaced conventional solutions for cardiovascular diseases. Innovative devices have been created for chronic pacing or programmed termination of arrhythmias, which have advantages over traditional options such as their flexibility and minimally invasiveness.
Diagnostics, Neurotechnology, and Optogenetics
Recent research predicts that photonics will be utilized in more than 20% of diagnostic tests by 2035, and they may play a key role in enhancing the efficiency and efficacy of diagnostic testing. The COVID-19 pandemic highlighted the importance of optics in diagnostics, with each one of the UK’s daily PCR tests being read via laser technology. While optics had been key to diagnostics prior to this, the pandemic emphasized their importance.
Photonics-based instruments currently account for £2.5 billion of the UK’s national healthcare system each year, equating to 4% of its total budget. This figure is predicted to rise over the coming years, with the benefits of optical solutions, such as their affordability and efficiency, leading to further use of photonics over traditional testing which is generally considered to be unsustainable and unaffordable in the long term.
By 2035, it is predicted that advances in integrated photonics will have allowed testing that currently requires laboratory-sized instruments to be carried out on miniature chips. This will change the face of diagnosis, with testing being brought to the bedside, into the operating theater, and the GP’s surgery.
Light will change the face of both medical diagnostics and treatment; it will allow scientists to gain important insights into the nature of the disease and how it affects different people.
Implantable optogenetic devices are increasingly important to medical research and medical advancement over the next decade or so. They are already being used in research, particularly investigating diseases that affect the brain.
The development of optogenetic devices is opening up a new branch of neurotechnology that utilizes optical brain-computer interfaces. The field could potentially provide new therapeutic approaches to chronic conditions as well as lowering the cost of care. Below, we detail how the technology may be implemented to treat Parkinson’s disease.
Explained: Optogenetics
Video Credit: Massachusetts Institute of Technology (MIT)/YouTube.com
Using Optogenetics to Treat Parkinson’s Disease
The gold standard for treating Parkinson’s Disease is medication. The compound within the drug, which is the most potent medication for Parkinson's disease, alleviates the key symptoms of the disease, such as stiffness and slowness of movement by increasing dopamine levels in the brain. However, the drug has major side effects, such as dyskinesia and the development of impulsive behaviors. The impact of the drug also wears off over time.
Given that more than 10 million people worldwide are estimated to be living with Parkinson’s disease, there is an urgent need for more effective therapy. The current alternative treatment is surgical therapy with deep brain stimulation, which shows great promise. However, only a small proportion of Parkinson’s patients receive this therapy.
Studies have shown that deep brain stimulation can effectively treat motor impairment and it has also been shown to be effective at extending the effective window. While it is not without its side effects, such as those relating to mood and cognition, brain stimulation therapy represents a promising therapy area to explore.
Scientists are now trying to optimize brain stimulation treatment via the use of optogenetics. It is hypothesized that optogenetics could elucidate important gaps in our knowledge of Parkinson’s disease so that scientists can provide an enhanced, patient-specific therapy option.
More research in this field is needed before optogenetics reaches its full potential. In the coming years, it is likely that we will see more important breakthroughs from studies using implantable optogenetic devices, with the area of neurological diseases likely to gain the most benefit at first.
References and Further Reading
2019. Micro-scale implants inside the brain to cure Parkinson’s Disease. [Online]. European Commission. Available at: https://digital-strategy.ec.europa.eu/en/news/micro-scale-implants-inside-brain-cure-parkinsons-disease Accessed February 2022
Madrid, M., Brennan, J., Yin, R., Knight, H. and Efimov, I., 2021. Advances in Implantable Optogenetic Technology for Cardiovascular Research and Medicine. Frontiers in Physiology, 12. https://www.frontiersin.org/articles/10.3389/fphys.2021.720190/full
UK PHOTONICS 2035: The Vision. [Online]. UK Photonics. Available at: https://photonicsuk.org/wp-content/uploads/2021/10/Photonics_2035_Vision_Web_1.0.pdf Accessed February 2022
Zemelman, B., Lee, G., Ng, M. and Miesenböck, G., 2002. Selective Photostimulation of Genetically ChARGed Neurons. Neuron, 33(1), pp.15-22. https://www.cell.com/neuron/fulltext/S0896-6273(01)00574-8?
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.