A recent article published in Leukemia proposed a novel and simple technique for detecting and diagnosing myeloproliferative neoplasms (MPN) using immunofluorescence microscopy on blood smears.
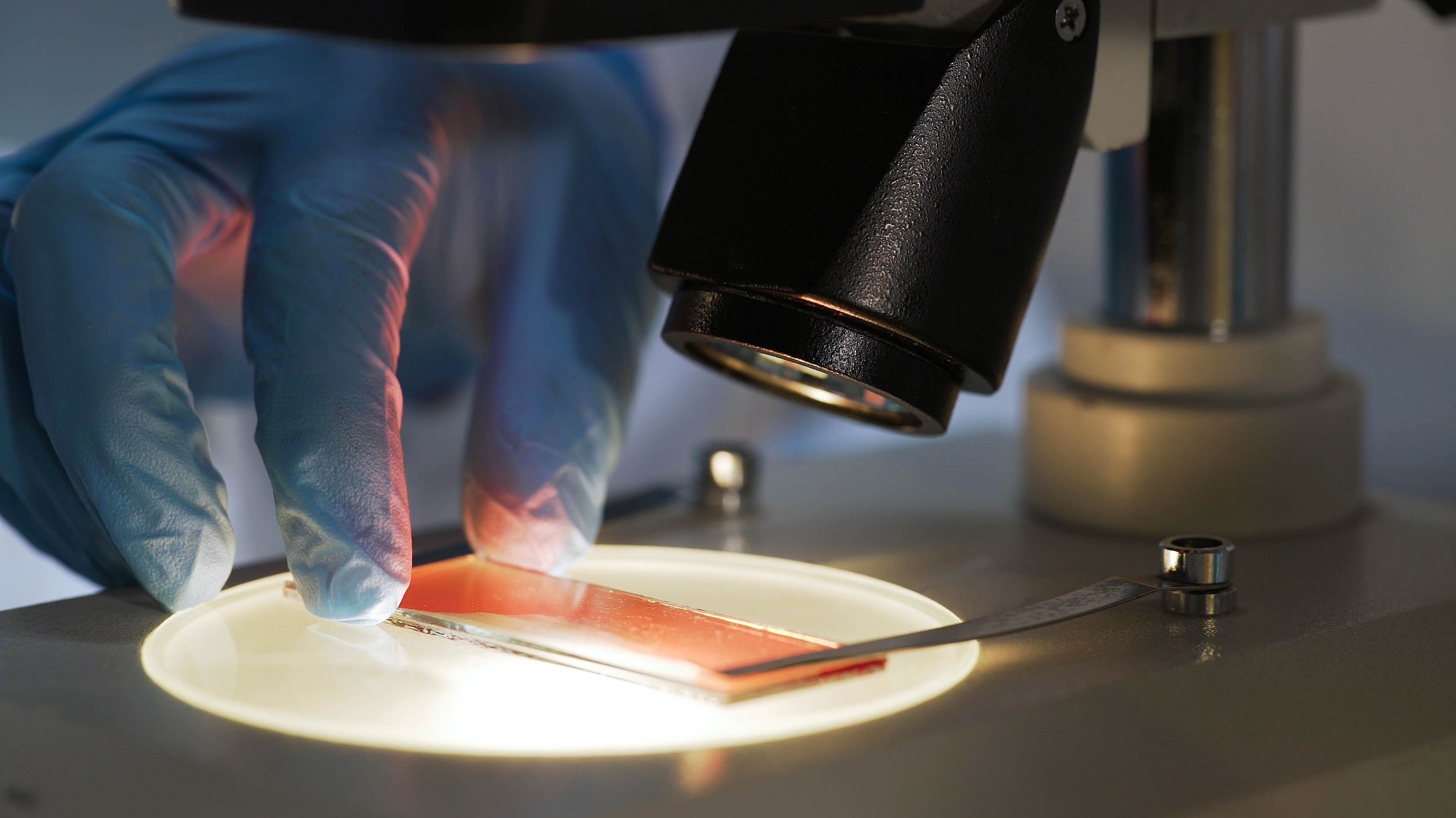
Image Credit: Motortion Films/Shutterstock.com
This method requires minimal blood samples and equipment. The researchers aimed to address the need for early diagnosis and treatment of MPN, which is crucial to prevent complications such as thrombosis and disease progression.
MPN Blood Disorders
MPNs cause abnormal growth of blood cells, leading to complications like thrombosis, bleeding, and other disease progression. MPNs include polycythemia vera, essential thrombocythemia, primary or secondary myelofibrosis, and unclassifiable MPN. Diagnosis relies on clinical, hematological, and molecular criteria defined by the World Health Organization (WHO).
However, molecular testing to detect somatic mutations in genes like Janus Kinase 2 (JAK2), calreticulin (CALR), and myeloproliferative leukemia (MPL), present in most MPN patients, is not widely available or affordable in many countries. Therefore, alternative, easy-to-apply diagnostic tools are needed to identify MPN patients and assess their risk of complications and disease progression.
State-of-the-Art Platelet Disorder Technique
Immunofluorescence microscopy uses fluorescent antibodies to label specific structures or molecules on cells, making them visible under a microscope. The researchers previously used this technique to diagnose inherited platelet disorders by identifying disease-specific changes in platelet shape and function. These rare disorders affect the number and function of platelets, which help with clotting and wound healing.
The study also reported that some patients with inherited platelet disorders have aggregates of a cytoskeletal protein called non-muscular myosin IIA (NMMIIA) in their red blood cells (RBCs), indicating abnormal red blood cell production (dyserythropoiesis).
About the Research
In this study, the authors assessed platelet and red blood cell (RBC) features using immunofluorescence microscopy in 135 MPN patients and 83 healthy subjects. They used a panel of antibodies to label 13 structures, including alpha and dense granules, platelet surface receptors, cytoskeletal proteins, the stem cell antigen CD34, and NMMIIA in RBCs.
A blinded, semiquantitative analysis of the blood smears was performed, with a grading system assigned to the morphological changes. Additionally, light microscopy and molecular testing were used to confirm the diagnosis and genotype of the patients.
Research Findings
The researchers highlighted that immunofluorescence microscopy revealed two distinctive features in MPN patients that were not present in healthy individuals: aggregates of NMMIIA in RBCs and reduced expression of platelet alpha granule markers.
NMMIIA controls cell shape and movement, and its aggregation in RBCs indicates abnormal red blood cell production. Platelet alpha granules contain various proteins involved in blood clotting and inflammation, and their reduced expression suggests impaired platelet function.
The study revealed that 98 out of 135 MPN patients (73 %) had aggregates of NMMIIA in their RBCs. Among these patients, 68 (approximately 69 %) showed reduced expression of at least two platelet alpha granule markers. Only 16 MPN patients (12 %) had normal immunofluorescence microscopy results.
None of the healthy controls exhibited NMMIIA aggregates or decreased expression of more than one platelet alpha granule marker. Other structural abnormalities were less significant, with only 7 MPN patients (5 %) showing changes in the platelet cytoskeleton and/or dense granules.
MPN patients with both altered platelet and RBC features had the highest levels of MPN driver mutations, such as those in JAK2, MPL, or CALR genes. These patients also had the highest prevalence of additional non-driver mutations, associated with an increased risk of disease progression.
Conclusion
In summary, immunofluorescence microscopy of peripheral blood smears proved to be an effective, clinically useful, and straightforward diagnostic tool for identifying MPN patients.
This method could be valuable in low-income countries with limited access to molecular testing and as a preliminary screening tool in high-income countries before performing next-generation sequencing. It could help understand the pathogenesis of MPN and the link between somatic and germline mutations in blood disorders.
Moving forward, researchers acknowledged limitations such as the retrospective design, heterogeneity of the patient population, and lack of correlation with clinical outcomes. They suggested validating the method in larger, prospective cohorts, investigating the mechanisms underlying the morphological changes in platelets and RBCs, and evaluating the prognostic value of this approach in MPN patients.
Journal Reference
Zaninetti, C., et al. (2024). Immunofluorescence microscopy on the blood smear identifies patients with myeloproliferative neoplasms. Leukemia. DOI: 10.1038/s41375-024-02346-
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.