New “maps” of hundreds of thousands of cells linked to inflammatory bowel disease (IBD) provide newer insights on their effects on intestinal tissues via a newly employed imaging method known as “imaging mass cytometry.”
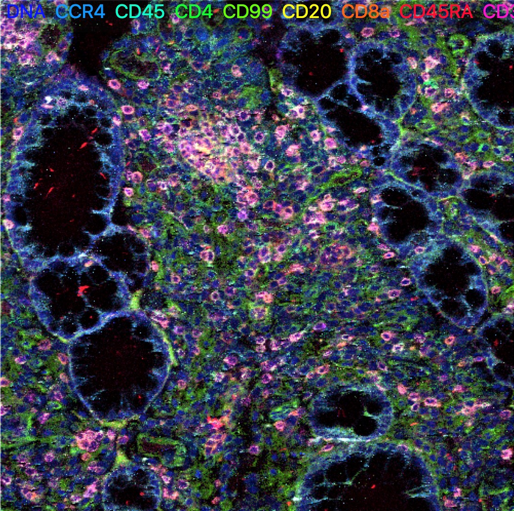 Multi-color image of a colon from a patient with ulcerative colitis stained by imaging mass cytometry. Image Credit: Dr. Ayano Kondo from the Kaestner lab.
Multi-color image of a colon from a patient with ulcerative colitis stained by imaging mass cytometry. Image Credit: Dr. Ayano Kondo from the Kaestner lab.
The innovative findings by scientists at the Perelman School of Medicine at the University of Pennsylvania offer a promising path to better targeted and more customized methodologies for treating IBD. Details of the research have been published in Gastroenterology.
IBD is projected to impact approximately seven million people worldwide and is an umbrella term that covers numerous disorders relating to inflammation of the gastrointestinal tract. The majority of cases are of ulcerative colitis or Crohn’s disease, which have varied clinical presentations and tend to impact the gut in diverse patterns. However, there is sufficient symptom overlap that the two diseases can be challenging to differentiate.
Treatments targeting particular immune signaling pathways exist for both disorders, but they do not function in the same manner with every patient and can have unfavorable side effects, including increased danger of infections.
To develop better treatments and better ways of diagnosing IBD we need to gain a more complete understanding of this set of disorders at the cellular and molecular level, and this study demonstrates a powerful new way of doing that.
Klaus Kaestner, PhD, Study Senior Author and Professor in Genetics, University of Pennsylvania
Conventional pathology procedures have their limits in what they can expose in biopsied intestinal tissue from patients with IBD. This is because they can quantify only a few protein markers, making it challenging to fully differentiate all pertinent cell types.
Alternatively, imaging mass cytometry uses a group of specially engineered antibodies that bind to over 30 distinct antigens — the molecular substances that activate the body’s immune response — allowing scientists to map all cell types in a particular patch of tissue at high resolution.
Kaestner’s team, including first author Ayano Kondo, a graduate student in his laboratory who carried out most of the analyses, applied the new imaging technique to six intestinal tissue samples from patients with Crohn’s disease and six from patients with ulcerative colitis, comparing these to samples from healthy people.
The cellular map outputs, the first of this kind in IBD research, encompassed hundreds of thousands of individual cells — and offered a number of new details of how IBD disturbs the stability of intestinal tissue.
Intestine-lining epithelial cells, for instance, were increasing more quickly in the IBD tissue compared to healthy tissue and were more probable to express the immune system component HLA-DR, which can help trigger an inflammatory reaction by the immune system. These properties matched with the degree of inflammation in both diseases.
The mapping also specified the occurrence in the diseased tissue of T-reg cells — regulatory immune cells that typically help moderate inflammation — and suggested that between ulcerative colitis and Crohn’s disease, there are definite variances in the patterns of other immune cell types with which T-reg cells interact.
On the whole, these findings give us new leads to pursue in understanding IBD, in defining sub-groups of patients who could benefit from more personalized treatments, and in developing new treatment approaches.
Klaus Kaestner, PhD, Study Senior Author and Professor in Genetics, University of Pennsylvania
The study was financially supported by the National Institutes of Health (R37 DK053839).
Journal Reference:
Kondo, A., et al. (2021) Highly multiplexed image analysis of intestinal tissue sections in patients with inflammatory bowel disease. Gastroenterology. doi.org/10.1053/j.gastro.2021.08.055.