Apr 10 2019
Schizophrenia and Alzheimer’s disease are some of the most widespread brain maladies and have been linked with issues in cells that hold a type of protein, known as parvalbumin. These parvalbumin-containing cells account for nearly one-tenth of the cells in the brain, however, comparatively little is known about the function of parvalbumin cells. By triggering mouse brains with lasers, scientists have begun making astonishing findings of their function.
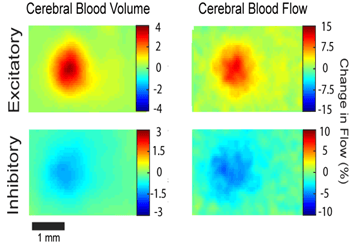 Using their custom-built laser system, researchers in the Bauer Lab at Washington University in St. Louis discovered that increased activity in specific inhibitory neural circuits reduces cerebral blood flow and volume while excitatory activity causes blood flow and volume to increase. (Image credit: The Bauer Lab at Washington University in St. Louis)
Using their custom-built laser system, researchers in the Bauer Lab at Washington University in St. Louis discovered that increased activity in specific inhibitory neural circuits reduces cerebral blood flow and volume while excitatory activity causes blood flow and volume to increase. (Image credit: The Bauer Lab at Washington University in St. Louis)
Scientists in the lab of Dr. Adam Q. Bauer, at Washington University in St. Louis, U.S.A., have discovered amazing variations in blood volume and flow when parvalbumin-containing cells are stirred. The method they used depends on specially bred mice whose brains can be triggered with laser pulses. They will present the results the OSA Biophotonics Congress: Optics in the Life Sciences meeting in Tucson, Arizona., U.S.A., between April 14th and 17th, 2019.
One of the key types of the brain’s inhibitory cells, parvalbumin-expressing cells have been found to be accountable for maintaining the infinite signals of the brain in sync. Since appropriate nervous system development depends on nerves continually firing in concert with one another over time, performing this neural symphony has been found to be a vital part of controlling the connections between brain cells that enable them to form normally.
The method of exciting the brain with light signals, known as optogenetics, has offered huge insights into how the brain functions, including how the brain processes fear and the sense of smell, or what makes a person to become addicted to drugs.
“Optogenetics is convenient, less invasive and repeatable,” Joonhyuk Lee, one of the Bauer group scientists said. “And it’s more straightforward. You don’t have to stick any probes into mouse brains or anything.”
First, the scientists bred mice that exhibited a special, light-sensitive protein known as channelrhodopsin throughout the brain. Channelrhodopsin was initially found in algae, but researchers can use it to choose which parts of a mouse brain to switch on. When the right colored laser hits a particular area of the mouse brain, a desired neural circuit can be activated.
For comparison, the team bred mice that had channelrhodopsin stuck to parvalbumin-expressing neurons and mice with channelrhodopsin on excitatory Thy1-expressing cells. With each group, they were able to trigger the mouse brains with lasers and compare the results.
When most neurons are triggered, Lee said, the brain offers them with additional blood and oxygen. This occurred with the excitatory Thy 1 cells, but the lab’s results in relation to blood flow and volume showed the opposite response when parvalbumin-expressing cells were triggered.
How activity in specific neural populations is coupled to local changes in blood flow is fundamental to understanding how the brain regulates its blood supply.
Joonhyuk Lee, Dr. Adam Q. Bauer group scientist, Washington University, St. Louis.
The researchers established that parvalbumin-expressing cells have a way of pulling back and tweaking the blood supply in areas where they are stimulated.
Scientists measured the oxygen and blood levels by shining a separate laser system, known as laser speckle contrasting imaging, on the brain. When the whiskers of the mice were touched, Lee and his colleagues first learned that parvalbumin cells could scale down nearby available blood and oxygen when stimulated. The team then measured various areas of the brain and found that parvalbumin cells could help transmit messages to distant corners of the brain to alter their hemodynamics, or blood flow, as well.
We really weren’t expecting that activation of parvalbumin-expressing neurons would result in a reduction of local blood flow and volume. Even more so, although it could be an indirect cause, the fact that we saw similar hemodynamic activity in more distant areas of the brain was very surprising.
Joonhyuk Lee, Dr. Adam Q. Bauer group scientist, Washington University, St. Louis.
Ultimately, Lee said, he hopes the findings and methods will help pave the way to a better understanding of parvalbumin’s function in neurovascular coupling and offer another piece of the puzzle on how it impacts brain development or development of neurological disorders.